
Risks Of Manual Hospital Systems: Hidden Patient Safety Threats You Can’t Ignore
Medication errors are among the most common medical errors in healthcare, with the costs of treating drug-related injuries in hospitals amounting to $3.5 billion annually. The risks of manual hospital systems extend far beyond financial implications, creating serious threats to patient safety that cannot be overlooked. In fact, the frequency and consequences of iatrogenic injuries (those caused by medical treatment) dwarf the frequency of other types of injuries that have received more public attention, such as airplane and automobile crashes.
Hospital pharmacy management is particularly vulnerable to error, as a recent meta-analysis reported an overall incidence of 6.7% for serious adverse drug reactions in hospitals. What makes this statistic even more concerning is that between 28% and 56% of adverse drug events are preventable.
Medication management in hospitals involves a complex process from prescription to administration, requiring coordination among multiple healthcare professionals. Consequently, manual processes in healthcare create numerous opportunities for human error, with potentially devastating outcomes for patients.
Hospital automation systems, particularly hospital pharmacy automation, significantly contribute to reducing medication errors, strengthening traceability, optimizing inventory management, and alleviating the workload of healthcare professionals.
Manual Processes in Healthcare: Where Things Go Wrong
Healthcare facilities worldwide continue to rely on manual processes that create significant patient safety risks. According to The Joint Commission, poor communication contributes to over 60% of all hospital adverse events in the USA. This sobering statistic reveals how outdated manual systems compromise care quality through various interconnected failure points.
Unstructured Communication Between Departments
Ineffective communication between healthcare departments represents a major weakness identified by risk managers. When patients transfer between units, the potential for incorrect information transmission or missing details constitutes a serious safety hazard. Unstructured conversations during patient handoffs often contain vital information necessary for continuity of care.
Furthermore, communication failures during transfers frequently lead to delays in diagnosis and treatment, ultimately resulting in adverse events.
This problem becomes particularly acute during transfers between intensive care units and general wards, where multiple activities occur simultaneously in chaotic environments. Without structured communication protocols, critical information gets lost in translation, putting patients at risk.
Paper-Based Records and Lost Information
Despite technological advances, many healthcare facilities still depend on paper-based patient records that introduce additional risks. Studies reveal that parallel use of electronic and paper records results in troubling inconsistencies between the systems. These discrepancies force physicians to check both record types to review past complications and comorbidities.
Additionally, paper records create challenges through illegible handwriting, limited space for documentation, and difficulties with information transfer. Physicians and nurses struggle to share or retrieve information quickly when using paper charts, slowing decision-making and potentially jeopardizing patient outcomes. Moreover, paper records remain vulnerable to physical disasters like fires or floods, making critical medical information irretrievable when needed most.
Manual Inventory Tracking in Hospital Pharmacies
Hospital pharmacies face numerous inventory management challenges when relying on manual processes. Many hospitals still track supplies manually, with outdated inventory systems in different departments unable to communicate with each other. This lack of real-time visibility into pharmaceutical stocks leads to costly issues including last-minute ordering, stockouts, and overstocking.
In busy operating environments, clinicians often lack the time to scan entire supply rooms thoroughly or check product expiration dates. Manual tracking of such fluid inventory data becomes virtually impossible beyond a certain point. For pharmacy teams, these inefficient processes result in wasted time—hours spent counting and organizing inventory rather than focusing on patient care.
The Real Cost of Human Error in Hospitals
Human errors within hospital systems extend beyond simple mistakes to create profound, measurable harm. The financial burden alone is staggering—experts estimate preventable medical errors cost the healthcare system between USD 20 billion and USD 45 billion annually. However, the true costs transcend mere dollars and cents.
Patient Harm from Incorrect Dosage or Delayed Administration
The clinical impact of medication delays presents a sobering reality. In intensive care settings, patients experience an average delay of 88 minutes for stat medications. These timing failures directly translate to worsened patient conditions. Specifically, delaying vasodilators by just one minute increases a patient’s odds of developing hypertension by 2.99%, with a typical 45-minute delay increasing this risk by 134%.
Similarly, delaying bronchodilators by one minute raises the chance of respiratory distress by 1.06%. For critical medications like antibiotics, delays are particularly dangerous—mortality increases in sepsis patients with every hour antibiotics are delayed.
Regulatory Non-Compliance and Legal Exposure
Beyond patient harm, manual systems increase vulnerability to compliance failures. Healthcare organizations that fail to establish robust internal compliance systems face severe consequences: substantial financial penalties, contract termination, criminal prosecution, and reputational damage.
The repercussions of non-compliance affect patients first—over 37.5 million records were exposed in 64,180 data breaches in 2021 alone. Notably, patients who lose trust in their providers often withhold crucial information, leading to misdiagnoses and inappropriate treatments. This deterioration in care quality increases provider costs while reducing income from programs like the Hospital Readmissions Reduction Program.
Operational Inefficiencies and Staff Burnout
The cumulative effect of system inefficiencies manifests in workforce burnout. Approximately 1 in 3 physicians and advanced practice providers surveyed intended to reduce work hours, while 1 in 5 physicians and 2 in 5 nurses planned to leave their practice altogether. Burnout-related turnover costs reach approximately USD 9 billion for nurses and between USD 2.6 to USD 6.3 billion for physicians annually.
As an underlying cause, primary care physicians reported spending significant time on non-clinical compensatory labor like chasing missing information from hospitals or resolving technology malfunctions.
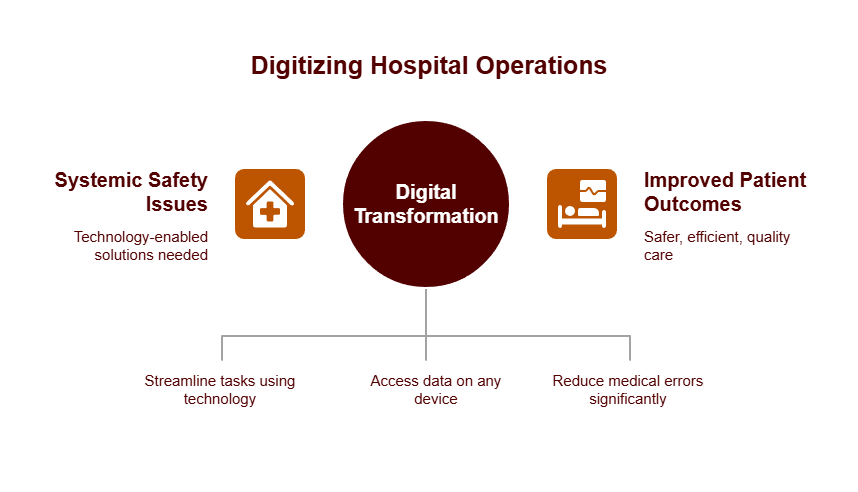
Digitizing Hospital Operations: A Strategic Imperative
Digital transformation in healthcare presents an unprecedented opportunity to address systemic safety issues through technology-enabled solutions. By implementing digital technology for innovative solutions, healthcare systems can achieve substantial improvements in care delivery and medical outcomes.
Healthcare Workflow Automation for Standardized Protocols
Workflow automation, which identifies sequences of tasks that can be streamlined using technology, directly addresses challenges with quality, safety, and efficiency. This approach reduces burden on providers, improves quality, and delivers better value to patients. Primarily, standardization enables reliable, high-quality care since it can be both measured and reproduced. Through automation, hospitals establish consistent triage, care escalation, and documentation protocols—essential in multi-site systems to guarantee standardized quality. Essentially, CPGs provide a basis for measuring provider performance and subsequent quality improvement initiatives.
Real-Time Data Visibility Across Care Teams
Real-time access to patient data revolutionizes clinical decisions and treatment. At Michigan Medicine, a cloud-based platform enables clinicians to access real-time data on any patient from anywhere using any connected HIPAA-compliant device. This elimination of paper-based processes generated savings while allowing staff to focus on direct patient care. Presently, unified dashboards display vital signs, metrics from devices, EHR data, clinical notes, and diagnostic results—all securely accessible 24/7.
Reducing Medical Errors with Automation Tools
Automation technology undeniably improves patient safety. Studies on bar-coding medication administration show 54-87% reductions in errors during medication administration. Correspondingly, CPOE systems demonstrate 55-83% reductions in medication errors. Following implementation of digital hospital systems including CPOE with CDSS, medication incidents decreased by 38%, and medication orders with errors dropped from 52.8% to 15.7%. Beyond safety improvements, automation enables clinicians to treat more patients in less time while substantially reducing hospital costs.
Implementing Automation: From Risk Mitigation to ROI
Successful automation implementation requires a methodical approach beyond merely selecting technology. Initially, organizations must evaluate existing workflows prior to digital transformation to ensure meaningful integration and sustainable results.
CyberMedics’ Custom Automation Development Process
CyberMedics collaborates directly with healthcare teams, mapping existing workflows and establishing clear objectives. Their process blends brainstorming, value-stream mapping, and human-centric design to blueprint custom applications.
Instead of offering temporary fixes, they provide tailored metrics and dashboards that deliver measurable, lasting improvements to business operations. Their comprehensive approach includes implementation planning, training materials, and ongoing system support to guarantee successful transitions.
Integrating Electronic Workflow Systems for Hospitals
Proper workflow integration begins with thorough assessments that help clinicians understand routine workflow patterns in their clinical settings. Thereafter, clinicians can modify implementation plans based on individual needs. Studies demonstrate that incorporating technologies like automated vital sign uploads and voice-recognition software significantly improves clinical workflow efficiency. Importantly, this integration must address interoperability challenges, as automation requires standardized data formats to reduce mapping needs and enable reuse of automation approaches.
Measuring Impact: Error Reduction and Time Savings
Organizations implementing healthcare automation typically report substantial returns. EHR integration eliminates duplicate data entry, reduces medical errors by 40%, and saves up to 25% in administrative costs.
Equally impressive, healthcare organizations with advanced data integration capabilities experience an average 25% increase in annual revenue. In one hospital, professionals spent 80% less time on data-related administrative tasks after implementing automation tools.
Overcoming Resistance: Training and Change Management
Successful implementation hinges on addressing change resistance through stakeholder engagement. Organizations should identify and empower “change champions” to advocate for automation benefits. Gradually introducing automation through phased implementation helps build momentum and trust through quick wins.
Proper education programs demystify automation as a supportive tool rather than a replacement for clinical expertise. Ongoing stakeholder feedback ensures systems remain aligned with evolving team needs.
Don’t wait for a preventable error to expose system weaknesses. Contact CyberMedics today to assess and automate your hospital workflows.
Conclusion
The risks tied to manual hospital systems are not hypothetical—they are persistent, measurable, and costly. From the $3.5 billion spent annually on preventable drug-related injuries to the 60% of adverse events linked to poor communication, the data is clear: manual processes introduce unacceptable levels of risk.
Patient safety is the most critical casualty. Delays in medication administration, even by minutes, are clinically proven to increase hypertension, respiratory distress, and mortality in sepsis patients. Compounding these issues are paper-based records, fragmented communication, and manual inventory tracking—all of which hinder timely, accurate care delivery.
Workflow automation provides a proven solution. Digital systems reduce medication errors by up to 87% using barcoding and up to 83% through computerized provider order entry. More importantly, automation enables hospitals to implement standardized protocols, increase real-time visibility, and drastically reduce human error across clinical and operational functions.
Healthcare organizations that commit to automation report substantial returns:
- 40% reduction in medical errors
- 25% savings in administrative costs
- 80% less time spent on manual data tasks
- Significant improvements in staff retention and patient outcomes
But successful transformation is not achieved through off-the-shelf software. It demands a methodical, strategic approach—beginning with a deep understanding of existing workflows and pain points, followed by the design and implementation of tailored digital systems that integrate seamlessly into hospital operations.
CyberMedics specializes in this transformation. Through our proprietary CyberProcess™, we partner with healthcare leaders to assess risk, design customized software solutions, and implement with precision—delivering measurable impact across safety, efficiency, and compliance.
Now is the time to act. The longer hospitals rely on manual systems, the greater the exposure to clinical, operational, and legal risk. The question is no longer if automation is necessary—it’s how quickly it can be implemented before the next preventable error occurs.
Contact CyberMedics today to begin modernizing your hospital workflows. Together, we can reduce risk, optimize care delivery, and protect what matters most—your patients.
FAQs
Q1. What are the main risks associated with manual hospital systems?
Manual hospital systems pose significant risks, including medication errors, communication failures between departments, lost or inconsistent patient information due to paper-based records, and inefficient inventory management in hospital pharmacies. These issues can lead to patient harm, regulatory non-compliance, and operational inefficiencies.
Q2. How do medication errors impact patient safety in hospitals?
Medication errors can have severe consequences for patient safety. Even small delays in medication administration can significantly increase risks. For example, delaying vasodilators by just one minute can increase a patient’s odds of developing hypertension by 2.99%. In critical cases like sepsis, every hour of delay in antibiotic administration increases mortality rates.
Q3. What benefits does healthcare workflow automation offer?
Healthcare workflow automation provides numerous benefits, including standardized protocols for consistent care quality, real-time data visibility across care teams, and significant reductions in medical errors. Studies show that bar-coding medication administration can reduce errors by 54-87%, while computerized provider order entry systems can decrease medication errors by 55-83%.
Q4. How can hospitals measure the impact of implementing automation systems?
Hospitals can measure the impact of automation through various metrics. These include reductions in medical errors (up to 40%), savings in administrative costs (up to 25%), and time saved on data-related tasks (up to 80% reduction). Additionally, healthcare organizations with advanced data integration capabilities have reported an average 25% increase in annual revenue.
Q5. What steps should hospitals take to successfully implement automation?
Successful automation implementation requires a methodical approach. Hospitals should start by evaluating existing workflows, engage stakeholders to overcome resistance, provide proper training and education, and implement changes gradually. It’s also crucial to work with experienced partners who can provide customized solutions and ongoing support to ensure sustainable results.
